The Link Between Diabetes and Alzheimer’s Disease
by Oscar Jan MS, RDNNews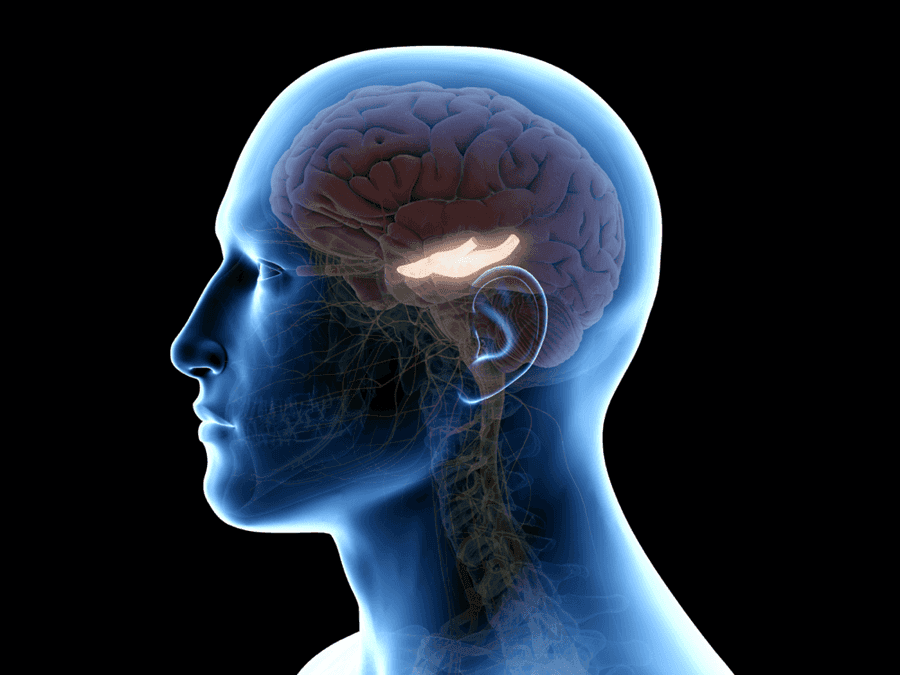
Alzheimer’s disease has long been considered a disease of the brain, but we now know that the pathology of Alzheimer’s extends beyond the brain and may be a result of systemic issues occurring in the rest of the body. In particular, a growing body of research has demonstrated a link between diabetes and Alzheimer’s disease. Diabetes is thought to contribute to a subset of Alzheimer’s disease known as glycotoxic Alzheimer’s. Glycotoxic Alzheimer’s, also referred to as Type 1.5 Alzheimer’s, is marked by inflammation as well as trophic withdrawal. Trophic withdraw refers to the insufficient delivery of vital nutrients or hormones to the cells, leading to cell dysfunction. In the case of glycotoxic Alzheimer’s disease, the brain is unable to utilize glucose for energy or respond to insulin signaling (1).
Diabetes occurs when blood glucose, or blood sugar, is elevated for prolonged periods of time (2). Normally, when blood glucose is elevated, the pancreas increases production of insulin, a hormone that helps transport blood glucose into the cells to be utilized for energy. In type 1 diabetes, the body is unable to produce sufficient insulin. In type 2 diabetes, the body may produce high amounts of insulin, but the cells are less responsive to insulin signaling, a process known as insulin resistance. As a result, glucose is unable to enter the cells and instead accumulates in the blood.
A number of epidemiological studies have demonstrated a correlation between diabetes pathology and Alzheimer’s pathology. One recent study conducted on 5,099 participants observed that late-life diabetes status, poor blood sugar control, and length of diabetes duration were all correlated with mild cognitive impairment (MCI); MCI often occurs during the early stages of Alzheimer’s disease and is a risk factor for Alzheimer’s (3). Furthermore, a meta-analysis conducted on 15 epidemiological studies found that type 2 diabetes increases the risk of developing Alzheimer’s disease by 57%, and this risk may be higher in those who carry the ApoE4 gene variant (4, 5). Magnetic resonance imaging (MRI) conducted on type 2 diabetes participants have also revealed anatomical changes similar to those observed in Alzheimer’s patients, such as decreases in hippocampal volume and cortical thickness (6,7). So why exactly might type 2 diabetes pathology contribute to the progression of Alzheimer’s disease? Research suggests that chronically high levels of blood glucose and impaired insulin signaling are two of the main mechanisms that may explain this link.
Insulin Resistance and the Brain
While insulin acts primarily on muscle and fat tissue, insulin can also cross the blood-brain barrier and influence how glucose is utilized by the brain, especially in the hippocampus, hypothalamus and cerebral cortex (1). Additionally, when insulin binds to insulin receptors outside of neural cells, it can signal a number of cascades within the cell related to memory, learning and synaptic plasticity (8).
Insulin signaling may also play a protective role against certain processes that contribute to Alzheimer’s disease. Insulin is involved in the regulation of a type of protein known as amyloid β (Aβ) (9). Excessive levels of Aβ can lead to the formation of plaques in the brain. These plaques can get in the way of neuron to neuron communication, leading to impairment in memory and thinking. Insulin signaling can prevent this process by reducing the accumulation of Aβ proteins. Insulin also helps maintain the structure of neural cells. Tau proteins are a group of proteins responsible for keeping neural cells stable. When tau proteins are phosphorylated, they clump and tangle up, resulting in the destabilization and death of neural cells. Insulin signaling can prevent these tangles from occurring by regulating the phosphorylation of tau proteins (1).
However, when insulin resistance occurs, insulin signaling is impaired. Impaired insulin signaling may result in dysregulation of Aβ processing and tau phosphorylation, contributing to the Aβ plaques and tangled tau proteins commonly associated with Alzheimer’s pathology. These plaques and tangles not only impair inter- and intracellular communication of neurons but can also promote inflammation in the brain, or neuroinflammation. Neuroinflammation may further exacerbate insulin resistance in the brain, resulting in a positive feedback loop.
Hyperglycemia, Oxidative Stress, & Inflammation
One of the hallmark characteristics of diabetes is hyperglycemia, or excess glucose in the blood. Hyperglycemia can result in the increased production of advanced glycation end products (AGEs), or molecules that form when proteins and lipids react with glucose (10). AGEs are often referred to as glycotoxins because of their ability to induce oxidative stress. Oxidative stress is particularly damaging to fat tissue, and since the brain is composed primarily of fat, high levels of oxidative stress can cause significant damage to the brain. Oxidative stress can also increase the expression of pro-inflammatory proteins such as IL-6 and TNF-α , resulting in neuroinflammation. Chronic neuroinflammation may trigger further production of Aβ plaques and tau tangles, resulting in further progression of Alzheimer’s disease (11).
Conclusion
Given the growing body of research linking diabetes with Alzheimer’s disease, maintaining control of your blood glucose levels is an important measure to prevent Alzheimer’s or slow down its progression. A healthy diet that is comprised of low glycemic foods and that minimizes simple carbohydrates can be helpful in keeping blood glucose under control. The addition of probiotic supplements or probiotic rich foods may also reduce inflammation and improve insulin sensitivity. Non-diet lifestyle habits that can positively impact blood sugar control include regular exercise, stress reduction, and getting adequate amounts of quality sleep.
The Bredesen Protocol incorporates all of these recommendations, along with additional interventions to regulate blood glucose, increase insulin sensitivity, and reduce inflammation. This integrative approach and recognition of the link between metabolic health and brain health may be some of the key factors contributing to the success of this program in reversing the signs and symptoms of Alzheimer’s. What is beneficial for overall health is also beneficial for brain health!
References:
- Kandimalla, R., Thirumala, V., & Hemachandra Reddy, P. (2017). Is Alzheimer’s disease a Type 3 Diabetes? A Critical Appraisal. Biochimica et Biophysica Acta, 1863(5):1078-1089. doi:10.1016/j.bbadis.2016.08.018
- Kharroubi, A. & Darwish, H. (2015). Diabetes mellitus: The epidemic of the century. World Journal of Diabetes, 6(6):850-867. doi:10.4239/wjd.v6.i6.850
- Rawlings, A.M., Sharrett, A.R., Albert, M.S., Coresh, J., Windhm, B.G., …Selvin, E. (2019). The Association of Late-Life Diabetes Status and Hyperglycemia With Incident Mild Cognitive Impairment and Dementia: The ARIC Study. Diabetes Care, 42(7):1248-1254. doi:10.2337/dc19-0120
- Vagelatos, N. & Eslick, G. (2013). Type 2 diabetes as a risk factor for Alzheimer’s disease: the confounders, interactions, and neuropathology associated with this relationship. Epidemiological Reviews, 35:152-60. doi:10.1093/epirev/mxs012
- Irie, F., Fitzpatrick, A.L., Lopez, O.L., Kuller, L.H., Peila, R., …Launer, L.J. (2008). Enhanced risk for Alzheimer disease in persons with type 2 diabetes and APOE epsilon4: the Cardiovascular Health Study Cognition Study. Archives of Neurology, 65(1):89-93. doi:10.1001/archneurol.2007.29
- Roberts, R., Knopman, D., Przybelski, S., Mielke, M., Kantarci, K.,…Jack Jr, C. (2014). Association of type 2 diabetes with brain atrophy and cognitive impairment. Neurology, 82(13):1132-1141. doi:10.1212/WNL.0000000000000269
- Moran, C., Beare, R., Wang, Wei., Callisava, M., & Srikanth, V. (2019). Type 2 diabetes mellitus, brain atrophy, and cognitive decline. Neurology, 92(8). doi:10.1212/WNL.0000000000006955
- Goncalves, R.A., Wijesekara, N., Fraser, P., & De Felice, F.G. (2019). The Link Between Tau and Insulin Signaling: Implications for Alzheimer’s Disease and Other Tauopathies. Frontiers in Cellular Neuroscience, 13:17. doi:10.3389/fncel.2019.00017
- Yamamoto, N., Ishijkuro, R., Tanida, M., Suzuki, K., Ikeda-Matsuo, Y. & Sobue, K. (2018). Insulin-signaling Pathway Regulates the Degradation of Amyloid β-protein via Astrocytes. Neuroscience, 385:227-236. doi:10.1016/j.neuroscience.2018.06.018
- Lee, H.J., Seo, H.I., Cha, H.Y., Yang, Y.J., Kwon, S.H. & Yang, S.J. (2018). Diabetes and Alzheimer’s Disease: Mechanisms and Nutritional Aspects. Clinical Nutrition Research, 7(4):229-240. doi:10.7762/cnr.2018.7.4.229
- DiSabato, D., Quan, N. & Godbout, J. (2016). Neuroinflammation: The Devil is in the Details. Journal of Neurochemistry, 139(Suppl 2):136-153. doi:10.1111/jnc.13607